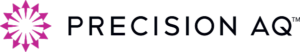
Proprietary Payer Data Master
State-of-the-art hierarchy and bridge files, updated in near real-time and connected to third-party, specialty, pharmacy, copay, hub and data sources
Reduce effort to connect the universe of complex healthcare data
- Establish a series of actionable, recognizable and differentiated payer names through three hierarchical levels for use across managed markets reporting platforms
- Provide a master payer spine and create a common definition of a payer for use across functional areas of a pharmaceutical company to allow meaningful integration of data across vendors
- Support all major forms of third-party vendor data via bridge files; bridge files also available for specialty pharmacy data
- Continuously review names and bridge files to capture the most current data available and appropriately classify payers in the most relevant manner, with updates delivered to client partners on a monthly basis
Third-Party Data Bridge
- IQVIA
- SYMPHONY
- MMIT
- BOT
- DRG
- CMS
- AIS
- BREAKAWAY
Unmask BIN-PCN-GROUP IDs and connect to the rest of your payer data universe

- First-of-its-kind, subscription-based translation service unmasks and connects complex payer information hidden in data sets
- Subscribers can immediately master BIN-PCN-GROUP identifiers contained in specialty pharmacy, direct reporting pharmacy, hub, copay and other healthcare data sources via our BPGLookup tool (run demo)
- Provides detailed channel descriptors for commercial health plans, employers, unions, worker’s compensation, ADAP, Medicare, EGWP, managed Medicaid, state Medicaid, and voucher programs
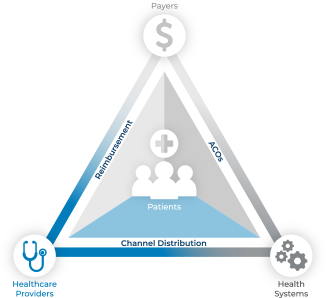
- Unlocks previously unattainable level of analytical insights to multiple stakeholders—including pharmaceutical manufacturers, specialty pharmacies, payers, data aggregators, PBMs, EMR vendors, and hospital systems
- Enables accurate measurement of transaction volume, the impact of data capture issues; helps control downstream delays in reimbursement
- Powered by Precision’s cross-asset data clearinghouse; governed and stewarded by a dedicated team of payer data experts

Start unmasking your data
Use an existing BIN-PCN-GROUP number and run a free test demo, on-demand!
Run demoContract Data Bridge

- Optimize payer marketing profitability; decode contract rebate formulary information to match bid grid for accurate analysis of contract
- Information from Rebate Submission Data
- Formulary Name deciphered from Enrollment Files
- Formulary Name translated to match published name
- Formulary matched to Bid Grid Groupings
BlueIndigo Data Management

- Account executives have ownership of formulary data flowing through the company
- Improve data accuracy with account manager override capabilities and preemptive changes to future values, based on account intelligence
- Experience significant savings in time and effort by replacing inefficient payer coverage-related communication across the organization
- 24/7 online tool
Let’s Talk
Drop us a line and one of our experts will be in touch with you right away.